Read an update on David Atkinson’s story here.
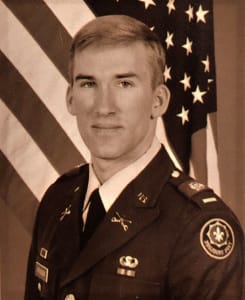
David Atkinson has lived his life in service: from West Point, to boots on the ground at Operation Desert Storm in 1991, to his free time spent as a volunteer for the National Ski Patrol. He’s always been “that” guy, the one you want to look over and find, by your side, in your most desperate of times… because you know he’s got this.
So in August of 2018, when David started feeling some mild pain in the back of his legs – it almost felt like a hamstring pull – he did the usual, the same thing many of us would have done: he sucked it up and pushed through the pain. For the next couple of months, the pain would come and go, but never fully went away. By early November, David was running a fever in the evenings and he sensed something more was awry than just a muscle pull.
One of the toughest things about prostate cancer is that it can be a silent killer. Prostate cancer is mostly symptom-free until it’s in its advanced stages. At that point, when it has likely spread to the lymph nodes and bones, it’s a lot easier to identify, and a lot harder to treat. By the time David finally decided to see a doctor in late November, his PSA came in at 350, about 500% above average for a man in his 50s.
David was sent straight to an oncologist. A bone scan revealed cancer metastasis in David’s right hip, the top of his right femur, his rib cage, and both shoulders.
When you spend half your adult life in the military, you envision yourself in a lot of tough situations. You spend time in your head strategizing your approach, your attack, your escape. You don’t spend a lot of time imagining a silent killer like prostate cancer. And you don’t spend a lot of time visualizing how you’ll tell your wife and your kids that you have stage 4 prostate cancer. “That was a tough conversation,” says David, with his signature, lionhearted mien, “Lots of tears.”
David was put on one of the standard of care drugs for his stage and type of cancer, abiraterone. Abiraterone is part of a newer suite of “androgen directed therapies” whose foundational research was funded by the Prostate Cancer Foundation to meet the needs of patients for whom standard ADT was no longer an option. David’s cancer did initially respond to treatment. “The good news,” says David, “is that treatments for advanced prostate cancer have come a long way. 6 years ago, my only option would have been chemo and a death sentence.” Over time, however, there was some bad news, as David had been warned when he started treatment: eventually, and often, the cancer learns to adapt and outsmart the drugs that are keeping it at bay. For David, that happened about a year after his diagnosis. That’s when he was referred to PCF-funded researcher Julie Graff at Oregon Health & Science University.
Initially, David was put on a phase 3 “combination therapy” clinical trial – using immunotherapy and a different androgen directed therapy than the one he had originally been on. Half of the men got the androgen receptor antagonist enzalutamide plus immunotherapy with pembrolizumab, and the other half got enzalutamide and placebo. On the trial, David’s PSA initially began decreasing. But this time, relatively quickly, it started going up. Some people might be thinking, “This is what I worry about with a clinical trial: what if I get the placebo and get worse, not better?” What most people forget is that on a clinical trial, the control group still gets the standard of care, not the proverbial “sugar pill.”
But in David’s case, the problem was that he had already had the standard of care, and his cancer had already evolved to evade it. Replacing one type of drug for another within the same class of therapy didn’t really solve David’s problem. Now he was in a race against time.
“Prostate cancer adapts to its environment,” says Graff. “It’s like a car engine – you can cut off the gas supply, but then the engine learns to keep running on a new fuel. What we needed to do was rebuild some parts of the engine.” Dr. Graff decided to sequence David’s tumor. Sequencing is the term that doctors use when they are examining the genetic code of the cancer, at a microcosmic level; based on what they find, doctors can come up with a precise treatment, termed precision medicine, that goes right for the jugular of the cancer. “What we’re looking for are clues as to where the defects might be in the engine, so we can target the exact sections that need rebuilding.”
Dr. Graff sent in a tissue sample from David’s original biopsy at diagnosis. The results indicated that his cancer would precisely respond to pembrolizumab. Since this was the drug from the other arm of the clinical trial, Graff immediately knew David had in fact been on the placebo arm of the trial and ordered immunotherapy; the FDA had already approved pembroluzimab for men with David’s tumor genetic profile. This type of immunotherapy, called an “immune checkpoint inhibitor” works by blocking the “off switch” of the immune system, allowing tumor-killing cells to attack the cancer.
Sometimes, finding the right drug for the right cancer is like looking for a needle in a haystack. But not this time: Graff knew the exact drug that David needed. They approached David’s private insurance company with the results of his tumor sequencing and asked if he could be taken off the trial and put directly on the trial drug – pembrolizumab – an exact match for his cancer. Twice they asked, and twice they were denied by the private insurance. Meanwhile, David’s condition was worsening.
That’s when Julie realized the path forward. “You’re a vet,” she said, “I’m the chief oncologist at the Portland VA. We need to get you over to there for your care.” David, however, was skeptical. “I was commissioned in ‘87. Back in the 80s, 90s? You heard all kinds of horror stories about VA medical care.” David enrolled at the VA and was served under the PCF-VA precision oncology program, designed to deliver the best and latest precision medicine to our nation’s heroes.
“I’m here to tell you,” says David, “in 2021, the VA quality of care is amazing, the staff is amazing, and I’m confident that they all have my best interests at heart.” The Prostate Cancer Foundation is proud to support PCF-VA Centers of Excellence around the country, delivering the best quality care to veterans with prostate cancer. PCF funding is allowing doctors like Julie Graff to do cutting-edge research and ensure that all veterans have access to the best treatments. David is now the VA’s biggest fan: “This is the best care you can get. Dr. Graff would not have known how to treat me if she didn’t have the PCF funding to do genetic testing and research. For folks like myself, I’m in a much better place because of the work PCF has funded.”
Exactly how much better? Just about two years after his initial diagnosis, David received one shot of pembro every three weeks for about four months. So far, the results have been positive. Dr. Jonathan Simons, President and CEO of the Prostate Cancer Foundation says guys like David are what it’s all about. “There have been so many drug advances for men with prostate cancer since we opened our doors in 1993. But we are not stopping at drugs that are less toxic; we are not stopping at drugs that are life-extending; we’re going full speed ahead until we find cures.”
“When I was first diagnosed around Christmas in 2018, I spent 4 days just lying on the couch. I was in so much pain that I couldn’t move. My wife and my sons had to do everything for me.” Now? “I’m at my desk and feeling pretty good,” says David. “I wouldn’t be here if it wasn’t for Dr. Graff and the PCF-VA Center of Excellence in Portland. And I’m so grateful.”
May is National Military Appreciation Month. If you would like to support PCF’s Veterans Health Initiative, please consider donating to the Veterans Health Fund.









